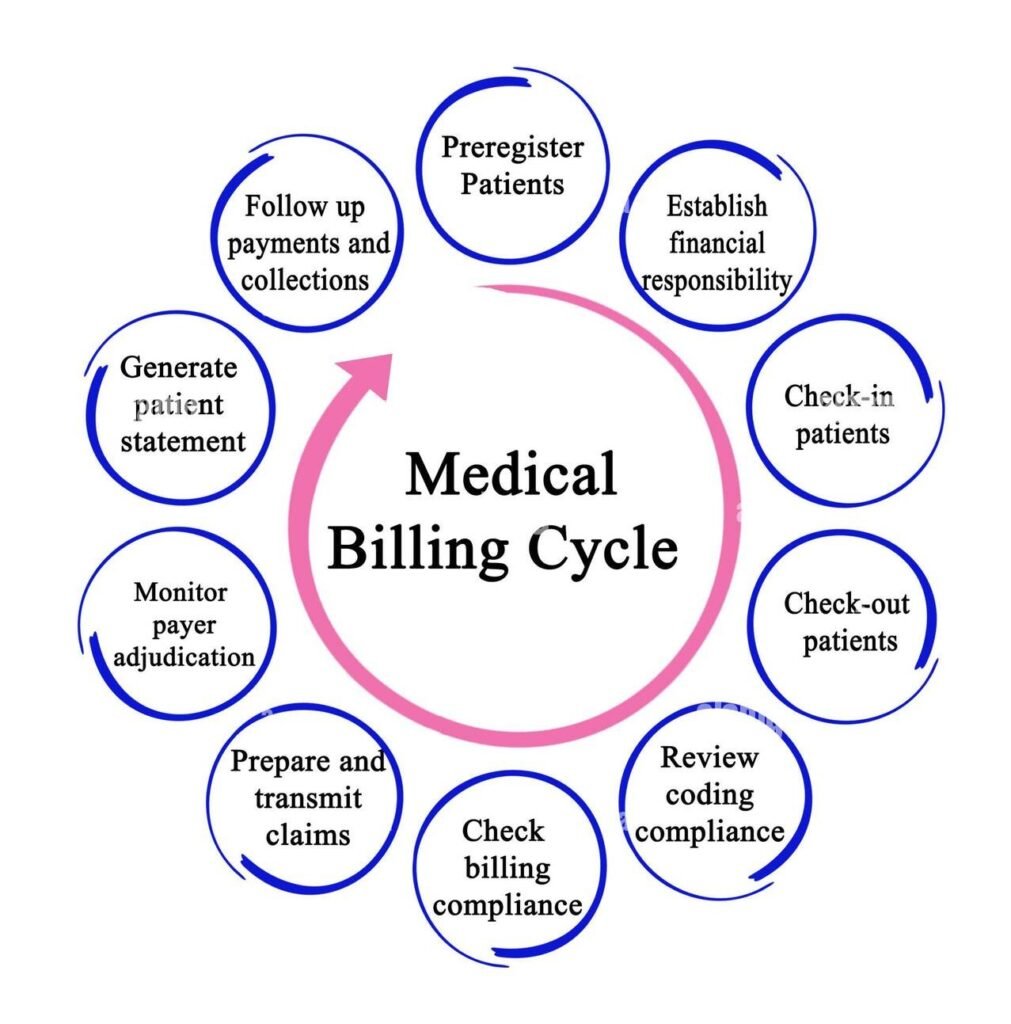
In the healthcare industry, medical billing is more than just submitting claims for payment. It is a structured process that directly affects the financial health of a practice and the satisfaction of patients. To run efficiently, a medical billing system relies on several interconnected components that ensure accuracy, compliance, and timely reimbursement. Understanding these components is essential for healthcare organizations, billing professionals, and anyone looking to optimize revenue cycle management.
Patient Registration and Data Collection
The first and one of the most crucial components of a medical billing workflow is patient registration. This is where the groundwork for the billing cycle is laid. Collecting accurate patient demographic details, insurance information, and medical history at this stage minimizes errors later on. Missing or incorrect information can lead to claim denials and delays, so precision here is critical. Practices often use automated systems to streamline registration and verify insurance eligibility in real-time, creating a smooth start to the billing process.
Insurance Verification and Authorization
Insurance verification ensures that the patient’s insurance policy is active and covers the planned services. Without proper verification, providers risk delivering services that won’t be reimbursed. Prior authorization from insurance companies for certain procedures also protects healthcare practices from claim rejections. This component is key to reducing financial risks and avoiding billing conflicts with patients.
Charge Capture
Charge capture involves recording all billable services rendered to the patient. This process requires close collaboration between healthcare providers and billing teams. Whether performed manually or through electronic health record (EHR) systems, accuracy in charge capture ensures that no service is left unbilled. Advanced billing systems can automatically pull procedure codes from provider notes, reducing human error and improving efficiency.
Coding of Medical Services
Medical coding translates diagnoses, procedures, and services into standardized codes like ICD-10, CPT, and HCPCS. These codes form the language of billing and insurance claims. This component of the workflow is critical for compliance with federal regulations and insurance requirements. Skilled coders ensure accurate representation of services, which directly impacts reimbursement rates and reduces the chance of audits or penalties.
Claims Submission
Once coding is complete, the claim is prepared for submission to the payer, typically electronically through clearinghouses. This stage requires strict attention to detail to ensure that all patient and service information is correct. Clean claims—those free of errors—speed up reimbursement, while claims with errors get denied or delayed. Effective claims submission also involves following payer-specific rules and timelines.
Payment Posting
After the insurance company processes the claim, payments are posted to the patient’s account. This step ensures transparency in the billing cycle and helps reconcile the amounts billed versus the amounts paid. Payment posting also identifies discrepancies quickly, allowing billing teams to follow up promptly with insurers or patients when necessary.
Denial Management and Follow-Up
Even with a flawless process, some claims are inevitably denied. Denial management is a vital component of the medical billing workflow that focuses on identifying reasons for denials, correcting them, and resubmitting claims. A proactive denial management system can significantly improve a practice’s cash flow and reduce bad debt.
Patient Billing and Collections
Once insurance payments are processed, any remaining balance is billed to the patient. Clear, transparent, and prompt patient billing helps improve collection rates and patient satisfaction. Offering multiple payment options, setting up online portals, and providing detailed billing statements create a positive patient experience and reduce disputes.
Compliance and Reporting
Compliance with HIPAA and other healthcare regulations is non-negotiable in medical billing. Protecting patient data, maintaining audit trails, and adhering to payer policies safeguard the practice from legal issues. Additionally, robust reporting systems allow healthcare providers to track performance metrics such as claim acceptance rates, days in accounts receivable, and collection efficiency. This data-driven approach supports informed decision-making and continuous improvement.
Technology and Automation in Medical Billing Workflows
Modern practices increasingly rely on technology to streamline billing processes. Automated tools for eligibility verification, coding assistance, and claim scrubbing reduce errors and speed up the billing cycle. Artificial intelligence and analytics platforms provide insights into trends and flag potential issues before they impact revenue. By integrating technology into each component of the workflow, organizations can achieve greater efficiency, compliance, and patient satisfaction.
Why Understanding Components Matters
Each component of the medical billing workflow is interconnected. Weakness in one area—such as inaccurate coding or delayed claim submission—can disrupt the entire revenue cycle. By understanding and optimizing each component, healthcare organizations can improve financial performance, enhance patient trust, and reduce administrative burdens on staff.
Conclusion
The components of a medical billing workflow work together like gears in a well-oiled machine. From patient registration to compliance reporting, every step plays a vital role in ensuring timely and accurate reimbursement. Healthcare providers who invest in training, technology, and process optimization will see smoother operations, stronger revenue cycles, and happier patients. In an evolving healthcare landscape, mastering these components is no longer optional—it is a necessity for sustainable growth.